Edward A. Cudahy and Eric L. Hanson
(Naval Submarine Medical Research Laboratory, Groton, CT 06349-5900)
Popular version of paper 2pBB2
Presented Wednesday afternoon, May 31, 2000
139th ASA Meeting, Atlanta, GA
Developments in the low-frequency active sonar systems used by the world's navies and by oceanographers have led to concern over the unknown health threats posed by underwater sound to divers who are exposed to these systems. Since sound underwater is perceived very differently from the way it is in air, simple extrapolation of noise exposure standards for airborne sound are clearly inappropriate to this problem.
The response of the human body to underwater sound is dictated by different physical principles than airborne sound exposures. The lungs are, probably, the most dramatic example of this. Like all body tissues, they are stiffer in compression and considerably denser than air. Yet, they are much softer and lighter than water. Other body tissue is roughly comparable to water or, like bone, is both denser and stiffer. Normally pressurized by the atmosphere, lungs may have an internal pressure equivalent to 5 or more atmospheres when a person is diving. These facts would lead a scientist familiar with the behavior of bubbles to predict a depth-dependent resonance caused by the motion of the lung against the mass of the surrounding water. If this vibration were undamped by body tissue, the motion of the lung might be amplified by as much as 100 times because of the resonance effect. What was not known until now was: does the human lung actually behave as if it were a bubble?
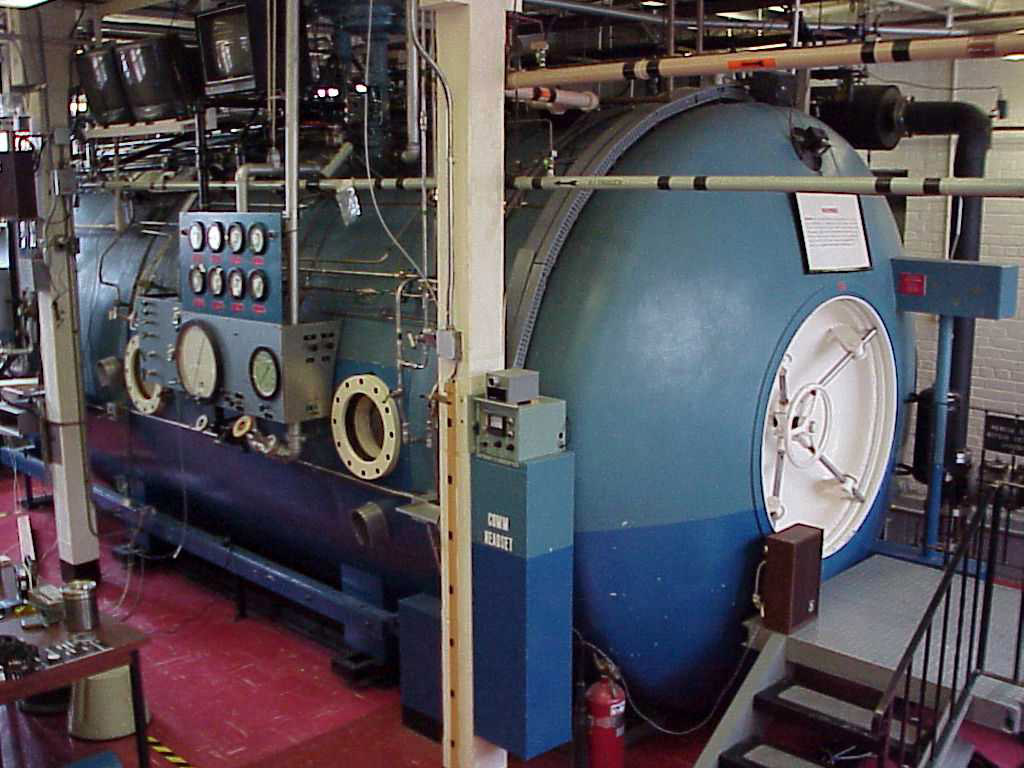
In order to answer this question, researchers from Georgia Tech and the Naval Medical Research Laboratory conducted an experiment in which volunteer navy divers were exposed to underwater sound in an 1100 gallon pool inside a large hyperbaric chamber which is normally used to treat decompression sickness. Varying the pressure within the chamber mimicked the effect of diving deeply without most of the associated risks. At each of 4 depths the motion of the divers' lungs were measured simultaneously using 3 different techniques during a sound exposure. To insure diver safety very low sound levels were used in the this experiment. These produced motions of a few millionths of an inch.
![]()
The results of the experiment reinforced the hypothesis that the lungs behave much like an air bubble. The measured lung resonances occurred around 39 Hertz (cycles per second) unpressurized and nearly doubled at a pressure equivalent to a depth of 120 feet of water. This was consistent with a lung whose stiffness was dominated by the air within. Due to damping from body tissue, the amplification of lung motion produced by the resonance was factor of 5 to 7. For those who have not experienced the Taos hum and do not recall (or choose to forget) Sensurround from the 1970s, 39 Hz is best described as the sound of a large diesel engine heard from a distance.
There are two ways in which the resonant amplification of lung motion could be dangerous to divers. Large motion might damage the lung itself or the lung might act as a secondary source of sound and cause damage to another organ system like the ear. The effects of resonant motion need not, however, be entirely negative. A project is currently underway in which researchers from Georgia Tech and Emory University are investigating the potentially therapeutic effects of low frequency underwater sound.
Oscillating chest compression is a common method for assisting cystic
fibrosis patients in clearing excess mucus from their lungs. Accomplishing
this compression with underwater sound offers many advantages over conventional
techniques such as pounding the chest wall. The number of oscillation cycles
which can be applied in a session is high (thousands per minute), the motion
produced in the lung is nearly uniform (this suggests that beneficial effects
will be provided to the entire lung rather than a small region of application)
, and large motions can be produced without injuring the patient. By exploiting
the lung's natural underwater resonance, the benefits of this therapy can
be achieved with substantially less input of energy. This has the dual
advantage of allowing the system to be more compact and providing an additional
margin of safety for the patients.