Thomas J. Royston - troyston@uic.edu
Xiangling Zhang, Hussein A. Mansy, Richard H. Sandler
Dept. of Mechanical Engineering
University of Illinois at Chicago
842 W. Taylor St. MC 251
Chicago, IL 60607
Popular version of paper 5aPPb13
Presented Friday morning, June 7, 2002
143rd ASA Meeting, Pittsburgh, PA
The pulmonary system consists of a network of airways, the bronchial tree, that start as one tube, the trachea, coming down through the neck into the chest and then split again and again into smaller and smaller airways which all terminate in the spongy part of the lung called the parenchyma. There are two parenchymae, one on our left and right sides. At these hundreds of thousands of tiny termination points the exchange of gases with the blood stream occurs, oxygen being absorbed and carbon dioxide being expelled. The parenchyma is spongy because it is full of air due to the many passage ways of the bronchial tree. We rely on an airtight chest cavity, airtight parenchyma and an airtight seal between them to hold the parenchyma (and thus its airways) open by suction. If the air pressure inside and outside of it are equal, each parenchyma would shrink to about the size of a fist closing off all but a few of the biggest more rigid airways close to the trachea.
This happens if there is a tear or puncture in the parenchyma and/or in the chest wall, and is known as a pneumothorax (PTX) or collapsed lung (Fig.1). Fortunately, the left and right parenchymae are in separate cavities so that if there is a tear on one side, the other side will not lose its suction. One collapsed lung is not as immediately life-threatening as both being collapsed but is still a very dangerous situation.
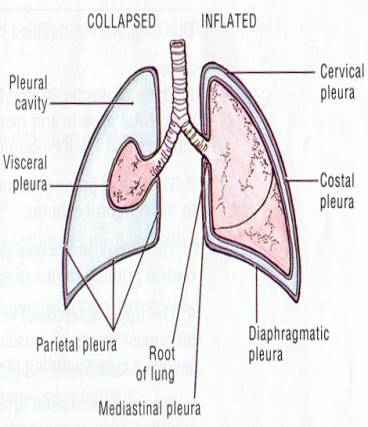
Fig. 1. Collapsed lung (Pneumothorax).
A collapsed lung can be caused by blunt or penetrating trauma that tears or punctures the chest wall or parenchyma, e.g. motor vehicle accidents, knife or bullet wounds, high-velocity ballistics and fragment wounds, blast injuries, or surgical procedures. Less frequently the parenchyma spontaneously tears creating a PTX. More frequently, such a tear can also occur when a patient is on a ventilating machine that cyclically forces air into the lungs using positive pressure. There are more than 20,000 PTX's each year in the U.S. and the cost of managing this condition is estimated at $130,000,000 by the American College of Chest Physicians. Because PTX's are life threatening, can be very fast paced, and are usually easily treatable, it is critical that the condition be rapidly diagnosed.
At present PTX diagnosis involves a combination of history, physical examination, and chest imaging procedures, typically a chest x-ray. The chest x-ray is usually sufficient for making a diagnosis; but, in the setting of critical illness, it may be difficult to obtain adequate positioning to enhance detection of the free air in the chest cavity. Furthermore, critically ill patients may not be movable to an x-ray computed tomography (CT) machine to allow enhanced detection capability. In addition, x-ray technology is not always available in remote or low technology settings.
An acoustic solution
Due to the collapse of airways and the creation of an air-filled cavity in the chest, one would expect that things might sound different. Physicians have recognized this. As the parenchyma pulls away from the chest wall and the airways collapse, breathing sounds diminish. But, many conditions requiring very different remedies can cause this; so, a qualitative recognition of this is not sufficient to make a diagnosis. Physicians have also noticed that the chest wall resonates more if tapped at the collar bone due to the free air space displacing the spongy parenchyma. But, these stethoscope-based techniques rely on the physician's skill, experience and good hearing, possibly in noisy environments, such as the ER, ambulance or battlefield.
The central hypothesis of our work is that a PTX leads to unique characteristic changes in sound transmission through the pulmonary system and this can be used to develop very inexpensive PTX-detection devices that are accurate, portable, rapid and safe.
Pilot study on dogs
In early studies we have done on healthy and PTX dogs, we have shown that PTX produces such a characteristic change in sound. Random noise with frequencies from 20 to 1600 Hertz with uniform amplitude was introduced into the entrotracheal tube at the mouth using a speaker. An electronic stethoscope measured the sound transmitted to the chest over the collapsed lung region. The average of the sound spectra of the chest responses in 15 dogs is shown in Fig. 2 for the baseline (no PTX) case and for a 30% PTX case (the parenchyma surface is separated from the chest wall by a distance that is about 30% of the total distance of separation for a completely collapsed lung).
Fig. 2 Average of the spectra of sounds transmitted from the mouth to chest wall of the 15 animals for the control (solid line) and 30% PTX (dashed line) states. A large drop is apparent in acoustic transmission due to PTX at frequencies above ~300 Hz. Note that the amplitude axis is logarithmic, so that the changes are a factor of 10-100.
Sample sound files are also given for normal and PTX cases. To hear typical
control (no PTX) sound, press here. To hear typical
30% PTX sound, press here. At low frequencies (f < 100
Hz), spectral values were about the same in the two states. However, at higher
frequencies (300 < f < 1200) the sound in the PTX cases was greatly reduced
in all animals. In order to reliably detect smaller PTX's, the methodology needs
improvement. A better understanding of the underlying acoustics and a means
of studying numerous alternative sensor and instrumentation configurations may
lead to improved detection ability.
Theoretical and computer simulation models of sound transmission
To better understand sound transmission in the chest, initial theoretical studies on very simplistic geometries were undertaken. A typical result using a 1-dimensional model of sound transmission from the center of the chest to the chest surface is shown in Fig. 3. This model approximates four components in the transmission path to the surface, the parenchyma, the air space if a PTX is present, the rib cage region and the outer soft tissue region. Qualitatively, similar trends to the dog experiments are seen.
Fig. 3 Theoretical prediction of acoustic response at the chest surface normalized to input pressure in the bronchial airway.
To gain a more precise simulation of the experiment finite element computer models are currently under construction. These models can use the geometry of actual subjects, or in the case shown below in Fig. 4, the National Library of Medicine's Visible Human Project, to derive extremely precise geometry based on x-ray CT scans or other imaging methods.
Fig. 4. Some preliminary images of conversion of NLM Visible Human project x-ray CT data to ANSYS Finite Element model for acoustic simulation.