Neb Duric- duric@karmanos.org
Peter Littrup, Earle Holsapple and Olsi Rama
Karmanos Cancer Institute, Wayne State University
Detroit MI, 48201
Popular version of paper 1pBB5
Presented Tuesday afternoon, November
28, 2006
4th ASA/ASJ Joint Meeting, Honolulu, HI
One woman in two receives a breast cancer scare in her lifetime. Each year over 250,000 women are diagnosed with breast cancer and over 45,000 die annually from the disease. Breast cancer continues to impact women's health and remains a major public health scourge. Mammography is currently the gold standard for breast cancer screening and diagnosis. Although a number of studies have demonstrated that mammography has saved lives, the reduction in death rates has been modest (15% to 30% according to most studies). Mammography's known limitations have prevented major breakthroughs in breast cancer survival rates. One major reason is that mammography presents a significant "false negative" rate, that is, it misses some cancers, particularly the smaller cancers in dense breast tissue.
Improving the false negative rate is important because early detection is crucial and can literally make the difference between life and death. In its earliest stages, breast cancer is highly curable but in the later stages it is a deadly killer. It is therefore critical to detect the cancer as early as possible. However, early cancers are small and often hard to detect by conventional means such as mammography. Therefore, the window of opportunity for treating the cancer at a curable stage is often missed.
A second problem is that mammography cannot easily differentiate between benign masses and cancer. Because the former are much more common, they end up causing a large number of cancer scares. Each cancer scare (false positive) arises from having to perform biopsies on benign masses. Biopsies can be painful procedures involving a partial removal of the breast, or at best, a needle that extracts a tissue sample. About a million biopsies of benign masses are performed in the US each year. The net result is a million cancer scares for women and billions of dollars of financial cost. Decreasing the false positive rate is the only way to reduce the biopsy rate and the staggering cost to the health care system.
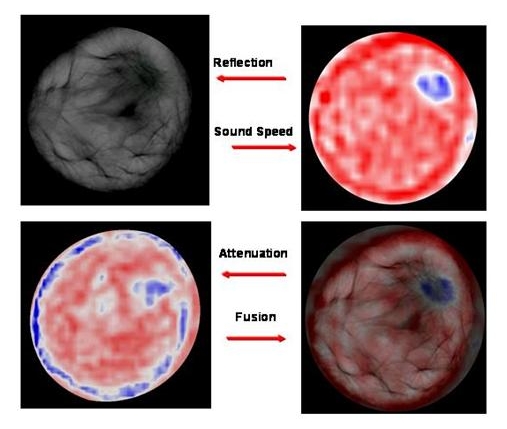
The high false positive and false negative rates associated with mammography justify exploring alternative techniques for breast cancer screening and diagnosis. Motivated by such considerations, we have been developing an alternative approach based on acoustical imaging. Perhaps the most familiar example of acoustical imaging in medicine is ultrasound. Currently, breast ultrasound is used as a follow-up to mammography but the duration of the ultrasound scan and its inability to view the whole breast has prevented its use in screening or in front-line diagnosis. We have extended the ultrasound concept by building an ultrasound imaging device that is, in effect, a CAT scanner of the breast. By surrounding the breast with ultrasound sensors we employ a technique known as "tomography", to produce sets of cross-sectional images of the breast that can then be assembled to provide a 3-D view of the breast's internal contents. This approach allows us to visualize a variety of acoustic properties of breast tissue that have the potential to (a) identify the small, hard to find cancers that are missed by mammography and (b) reduce the number of biopsies. Achieving these goals would increase the number of cancers caught in the curable stage and reduce the number of breast cancer scares.
Initial proof-of-concept tests of our approach suggest that we are on the right track. Based on the approximately 50 sets of patient data that we have analyzed thus far, we have shown that we can image reliably the internal contents of the breast and that we can measure those tissue properties that have the potential to differentiate cancer from benign masses. Furthermore, we have shown that we can do this without compressing the breast (a sometimes painful procedure associated with mammography) and without the harmful X-rays used by mammography. In our ongoing studies we will estimate the impact of our approach in improving the accuracy of breast cancer diagnosis and thereby explore the readiness of this approach for wide-spread use in the clinic.