2aBAb2 – Feasibility of using ultrasound with microbubbles to purify cell lines for immunotherapy application
Thomas Matula – matula@uw.edu
Univ. of Washington
1013 NE 40th St.
Seattle, WA 98105
Oleg A. Sapozhnikov
Ctr. for Industrial and Medical Ultrasound
Appl. Phys. Lab
Univ. of Washington
Seattle, Washington
Phys. Faculty
Lev Ostrovsky
Dept. of Appl. Mathematics
University of Colorado
Inst. of Appl. Phys.
Russian Acad. of Sci.
Boulder, CO
Andrew Brayman
John Kucewicz
Brian MacConaghy
Dino De Raad
Univ. of Washington
Seattle, WA
Popular version of paper 2aBAb2
Presented Tuesday morning, Nov 6, 2018
176th ASA Meeting, Victoria, BC, Canada
Cells are isolated and sorted for a variety of diagnostic (e.g., blood tests) and therapeutic (e.g., stem cells, immunotherapy) applications, as well as for general research. The workhorses in most research and commercial labs are fluorescently-activated cell sorters (FACS) [1] and magnetically-labeled cell sorters (MACS) [2]. These tools use biochemical labeling to identify and/or sort cells which express specific surface markers (usually proteins). FACS uses fluorophores that target specific cell markers. The detection of a specific fluorescence wavelength tells the system to sort those cells. FACS is powerful and can sort based on several different cellular markers. However, FACS is also very expensive and complicated such that they are mostly found only in large core facilities.
MACS uses magnetic beads that attach to cell markers. Permanent magnets can then be used to separate magnetically-tagged cells from untagged cells. MACS is much less expensive than FACS, and can be found in most labs. However, MACS also suffers from weaknesses, such as low throughput, and can only sort based on a single marker.
We describe a new method that merges biochemical labeling with ultrasound-based separation. Instead of lasers and fluorophore tags (i.e., FACS), or magnets and magnetic particle tags (i.e., MACS), our technique uses ultrasound and microbubble tags (Fig. 1). Like FACS and MACS, we attach a biochemical label (an antibody) to attach a microbubble to the cell’s surface protein. We then employ an ultrasound pulse that generates an acoustic radiation force, pushing the microbubbles; the attached cells are dragged along with the microbubbles, effectively separating them from untagged cells. This is accomplished because cells only very lightly interact with ultrasound, whereas microbubbles interact very significantly with the sound waves. We theorized that the force acts on the microbubble while the cell acts as a fluid that adds a viscous drag to the system (see [3]).

Figure 1. Cell separation technologies
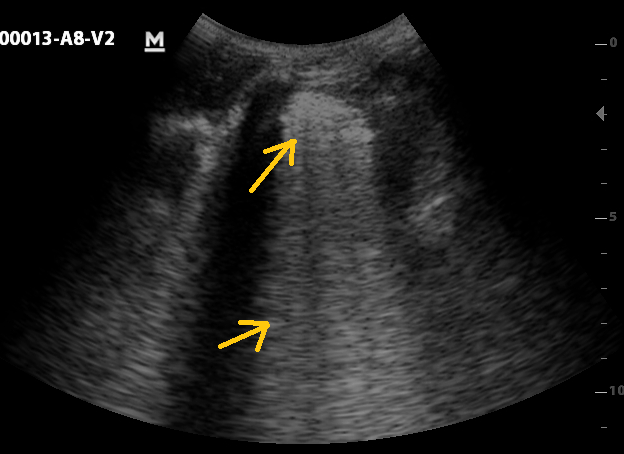
We can break down our studies into two categories, cell rotation and cell sorting. In both cases we constructed an apparatus to view cells under a microscope. Figure 2 shows a cell rotating as the attached microbubbles align with the sound field (the movie can be found by clicking here). We developed a theory to describe this rotation, and the theory fits the data well, allowing us to ‘measure’ the acoustic radiation force on the conjugate microbubble-cell system (Fig. 3).
 |
 |
 |
Figure 2. A leukemia cell has two attached microbubbles. An ultrasound pulse from above causes the cell to rotate.
| Figure 3. We assume that the microbubbles act as point forces. The projection of these forces perpendicular to the radiation force direction leads to a torque on the cell, which is balanced by the viscous torque. This leads to an equation of motion that can be put in terms of angular displacement. Thus, the parameters are detailed in [3]. The results are plotted along with the data, showing a nice match between the theory and data. For our conditions, the acoustic radiation force was found to be F=1.7×10-12N. | [IMAGE MISSING] |
When placed in a flow stream with other cells, the tagged cells can be easily pushed with ultrasound. Figure 4a shows how a single leukemia cell is pushed downward while normal erythrocytes (red blood cells) continue flowing in the stream (the movie can be found by clicking here). This shows that one can effectively separate tagged cells. However, in a commercial setting, one wants to sort with a much higher concentration of cells. Figure 4b illustrates that this can be accomplished with our simple setup (the movie can be found by clicking here).
To summarize, we show preliminary data that supports the notion of developing an ultrasound-based cell sorter that has the potential for high throughput sorting at a fraction of the cost of FACS.
| (a) [IMAGE MISSING] | (b) [IMAGE MISSING] |
Figure 4. (a) A single leukemia cell is pushed downward by an acoustic force while red blood cells continue to flow horizontally. It should be possible to detect rare cells using this technique. (b) For high-throughput commercial sorting, a much larger concentration of cells must be evaluated. Here, a large concentration of red blood cells, along with a few leukemia cells are analyzed. The ultrasound pushes the tagged leukemia cells downward. We used blue for horizontal flow (red blood cells) and red for ultrasound-based forcing downward.
[1] M. H. Julius, T. Masuda, and L. A. Herzenberg, “Demonstration That Antigen-Binding Cells Are Precursors of Antibody-Producing Cells after Purification with a Fluorescence-Activated Cell Sorter,” P Natl Acad Sci USA 69, 1934-1938 (1972).
[2] S. Miltenyi, W. Muller, W. Weichel, and A. Radbruch, “High-Gradient Magnetic Cell-Separation with Macs,” Cytometry 11, 231-238 (1990).
[3] T.J. Matula, et al, “Ultrasound-based cell sorting with microbubbles: A feasibility study,” J. Acoust. Soc. Am. 144, 41-52 (2018).