The
Sound Sleep Study: Building Evidence to Make Hospitals Quieter
Jo M. Solet - joanne_solet@hms.harvard.edu
Harvard
Medical School, Division of Sleep Medicine
and
Cambridge Health Alliance
Popular
version of paper 2aNSc1
Presented Tuesday morning, April 20, 2010
159th
ASA Meeting, Baltimore, MD
Noise in
health care facilities has increased by multiples in past decades. National
surveys in which patients assessed hospitals have shown that room noise levels
had ratings that were worse than other quality-of-care indicators. Individual
patient responses reflect this survey data.
Figure 1. Patient reactions
With rising
national healthcare costs and a wave of aging baby boomers on the horizon, greater
effort is being directed to the challenge of improving environments of care and the related health
outcomes.
The
Sound Sleep Study, at the interface of acoustics and sleep medicine, contributes
to this growing effort. Researchers from behavioral medicine, neuroscience, neurology,
biostatistics, and acoustics have come together to quantify the physiological impacts
of specific hospital-based sounds on human sleep.
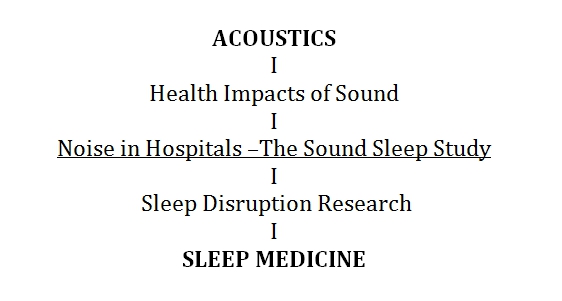
Figure 2. The Interdisciplinary Interface
Developing a Hospital Soundscape
First a
soundscape of a medical-surgical unit was developed
which included recordings at Somerville Hospital in MA. From this soundscape, 14 representative hospital noises were
calibrated to provide 10 second equal sound doses at increasing 5 decibel
step levels from 40 to 70 decibels on the A scale (adjusted for human hearing
sensitivity.)
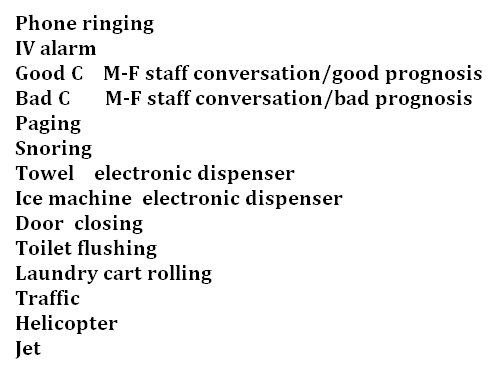
Figure 3.
List of Hospital
Sounds
Preparing the Sleep Lab for Sound
Playback
All
testing rooms in the Massachusetts General Hospital sleep laboratory have
monitoring equipment to measure brain activity and heart reactions during
sleep. For this noise protocol, one room was specially fitted with a surround
sound speaker system and a computer programmed to present dynamic replay of the
14 hospital sounds in random order at the rising noise levels .
Selecting Sleepers http://sleep.med.harvard.edu/research/recruitment
Twelve
adult subjects were selected from numerous responses to outreach advertisements
for research participation (see website above). Each participant was carefully screened
for normal hearing and for any health problems that could interfere with sleep.
Hospital Institutional Review Board and informed consent procedures were
followed as required.
Three Nights in the Sleep Lab
After
one quiet adaptation night, sounds were introduced on the two following
nights during bouts of stable sleep. Sounds were initiated at 40 dBA and
presented every 30 seconds in rising 5
dB increments until an arousal was observed or 70 dBA was reached. On all three
nights the subjects were physiologically monitored to indicate and record the
depth and stages of their sleep. This monitoring allowed for identification of arousals
(transition to a lighter sleep stage or full awakening) that followed immediately
upon exposure to the sounds.
Probability of Arousal
Arousal
information on all 12 subjects was combined for each of three sleep stages
separately: light sleep (NREM2), deep sleep (NREM3), and dream sleep (REM). The
percentage of subjects aroused by each of the 14 sounds at each decibel step level
was then plotted to form sleep stage specific arousal probability threshold curves. These combined results
confirmed that, at levels commonly experienced by patients, the selected
hospital sounds significantly disrupted sleep.
Intravenous
(IV) alarm and phone signals, designed to be alerting, showed the greatest
impact on sleep with between 88% and 94% of subjects aroused at the lowest
sound level of 40 dBA. Human voices, for which some
awareness during sleep could be adaptive, were also very arousing; between 70%
and 75% of subjects were aroused at 40 dBA. This finding
is consistent with patient complaints of sleep disturbance by night staff
conversations. No differences were seen between responses to conversations conveying
good or bad prognoses. Like speech, other sounds which had shifting contours, (Snoring,
Towel dispenser, Ice dispenser, Door closing and Toilet flush) produced higher
probability of arousal, between 35% and 73% of subjects at 40dBA, than those
which shifted less over the 10 second exposure periods. During dream sleep (REM),
there was less differentiation of sounds from each other in terms of arousal
impact than in light sleep (NREM2) or deep sleep (NREM3). Light sleep is the
most relevant for evaluating noise levels because greater time is spent in that
sleep stage for the adult population.
Implications:
For Hospital Design and
Construction
This
project contributes scientific evidence validating the provision of minimum
acoustic standards recently established in the 2010 edition of the Guidelines
for the Design and Construction of Health Care Facilities. The results also
underscore the need for innovation in materials and equipment to improve
acoustics in healthcare environments, positively impacting health outcomes
through improved sleep, privacy, and communication.
For Acoustic Science
Self-report
of satisfaction by the user is a common assessment tool for acoustic appraisal
of occupied buildings. However, self-report is not an adequate technique for
assessing sleep environments. During sleep, memory is not fully engaged, and subjects
often do not accurately remember arousal experiences. Even individuals who are aware of having
limited sleep underestimate the deficits in attention that result.
Our
evidence-based arousal probability threshold curves offer a clearer picture
of vulnerability to sleep disruption from noise. Accurate databases
contributing to acoustic assessments of sleep environments are critical for
protection of the health and functioning of noise-exposed residents.
For Sleep Medicine
This
research provides a methodology for bringing real acoustic elements into the
sleep laboratory, using fully monitored subjects to ascertain the probabilities
for arousal.
While
this project focused on healthcare facilities, disruption of sleep by noise occurs
in many environments, such as crowded urban neighborhoods and beneath airplane
flight-paths. More than just an annoyance factor, the health impacts over time
of disrupted sleep can be serious, including changes in glucose metabolism,
elevated blood pressure, increased inflammation, and higher risk of industrial
and auto accidents. Clear recognition of the role of noise in disrupting sleep
is necessary for policy decisions and code enactments to protect public health.
For Collaboration and Innovation
Reflecting
broadly on this innovative sleep and acoustics project, it is clear that solving
complex modern problems calls for greater permeability among disciplines. To engender
successful cross- disciplinary collaborations, foundations and touch points in
knowledge bases and standards of practice should be made more explicit. These encompass
critical concepts and heuristics, vocabulary and acronyms, reporting mechanisms,
and compensation systems. In addition greater transparency is needed regarding
conflicts of interest and sponsorship disclosures, client confidentiality requirements and human subject research
protections. There are also subtle,
often unspoken, characteristics of professional cultures, including the degrees
to which competitive individualism is endorsed, help seeking and error
detection are valued, hierarchy can be leveled, excellence defined, and real consensus
achieved.
Historically,
in the academic model, modest refinements within tightly defined scientific and
clinical fields have been most highly rewarded. To facilitate complex collaborative
problem solving in the future, new roles for boundary crossers and
interdisciplinary translators must be accorded higher value.
Acknowledgements:
Research Colleagues
From Harvard
Medical School, Division of Sleep Medicine
Orfeu M. Buxton, PhD Brigham and Womens Hospital
Jeffrey M.
Ellenbogen, MD Massachusetts General Hospital
Wei
Wang, PhD Brigham and Womens Hospital
With:
Andy
Carballeira, BM Berklee College of Music
Cavanaugh Tocci Associates, Inc
Research Sponsors
Center
for Health Design, Facilities Guidelines Institute, and Academy of Architecture
for Health.
Further Reading:
Solet, JM, Buxton, OM, Ellenbogen, JM, Wang, W, Carballeira, A,
Evidence-based design meets evidence-based medicine: The sound sleep study.
Concord, California, The Center for Health Design, 2010. (Executive Summary and Full Report)
http://www.healthdesign.org/resources/pubs/
The
American Society for Healthcare Engineering and The Facility Guidelines
Institute (2010). Guidelines for Design and Construction of Health Care Facilities 2010
Edition. Chicago, IL: The American Hospital Association.
Harris
DH, Joseph, A, Becker, F, Hamilton, KD, Shepley, MM,
Zimring,
C. A practitioners guide to evidence-based design.
Concord,
California, The Center for Health Design, 2008.
Joseph, A., & Ulrich, R. Sound control for
improved outcomes in healthcare settings (Issue Paper #4). Concord, CA: The Center for Health Design, 2007.
Bartick MC, Thai X, Schmidt T, Altaye A, Solet JM.
Decrease in as-needed sedative use by limiting nighttime sleep disruptions from
hospital staff. J Hosp Med. 2009 Sep 18. [Epub ahead of print] [PMID:
19768797] [print] 2010.
Busch-Vishniac, I.,
West, J., Barhnill, C., Hunter, T., Orellana, D., & Chivukula, R.
Noise Levels in Johns Hopkins Hospital. The
Journal of the Acoustical Society of America, 2005, 118, 3629-3645.
Jha, A., Orav,
E., Zheng, J., & Epstein, A. M. Patients
perception of hospital care in the United States. New England Journal of Medicine, 2008, 359,1921-31.
Gardner,
H. Five Minds for the Future
Harvard
Business Press, Boston, MA, 2008.
Harvard
Medical School, Division of Sleep Medicine subject recruitment: http://sleep.med.harvard.edu/research/recruitment
About the Presenter
Dr. Jo Solet is a member of the Division of Sleep Medicine at
Harvard Medical School and associated faculty at the Cambridge Health Alliance.
Her work as a clinician, teacher and researcher has focused on adaptation to
injury, illness, and disability. Recognizing that the physical context in which
patients recover may compromise or enhance their healing and ability to
function, she has been serving as principal investigator of a laboratory-based
research project with colleagues in acoustics and in the Division of Sleep
Medicine. This current project is a collaboration joining evidence-based
medicine with evidence-based design to understand the effects of noise on sleep
disruption in healthcare facilities. These findings have informed the Guidelines
for Design and Construction of Health Care Facilities 2010 Edition .