![]()
![]()
![]()
Shear Wave Elastography for
Detecting Blunt Force Trauma Liver Injuries
Jiao
Yu - jiaoy@u.washington.edu
Peter
Kaczkowski, Lawrence Crum, and Stuart Mitchell
Center
for Industrial and Medical Ultrasound, Applied Physics Lab, University of
Washington
Seattle,
WA 98105
Popular
version of paper 3aBB1
Presented
Wednesday morning, November 17, 2010
2nd Pan-American/Iberian Meeting on Acoustics, Cancun, Mexico
The
liver, the largest organ inside the body, can be injured by falling, or an
impact during a car accident or a sports related incident, due to its bulky
size and relatively fixed position in the abdominal cavity. Liver injuries can
be severe enough to be life-threatening because the liver has a large blood
supply and capacity; fractures of the liver or tears in the major hepatic blood
vessels present a serious risk for shock and even exsanguination.
Currently, a fast and robust way of visualizing hepatic fractures due to blunt
force trauma does not exist; hence, there is a need to develop better imaging
modalities of hepatic injuries to assist in clinical assessments in an
emergency room. In this study, we investigated the feasibility of using shear wave
elastography for detecting fractures of liver due to
blunt force trauma.
Shear
wave elastography is a new method to image and
characterize tissue structures based on the use of shear waves induced by the
focused ultrasound beams inside the tissue. Shear waves are different from
longitudinal waves (the waves that constitute sound). For shear waves, the
motion of the medium is perpendicular to the direction the wave is traveling.
Shear waves travel at a speed of 1-10 m/s, much lower than the typical longitudinal
waves (1540 m/s in tissue), and shear wave speed changes uniformly with the
elasticity of the local tissue region. Compared to the conventional ultrasound elastography, shear wave elastography
has mainly two advantages: It is more sensitive because the shear modulus
ranges over more orders of magnitude than the bulk modulus, which characterizes
longitudinal elastography; it is more localized and
less affected from tissue boundaries. Shear wave elastography
has been found to be useful in characterizing breast lesions and assessing
liver fibrosis.
We
also expect the shear wave elastography to be useful
in the detection of bleeding; for example, the shear wave can only propagate in
an elastic medium and thus it cannot propagate in fluids. When the shear wave
travels to the edge of a liver fracture, say, we expect to see a contrast at
the boundary of the fracture, where typically blood will present. To test our
hypothesis, an ultrasound beam was focused at different depths from 1 cm to 3.5
cm consecutively with a duration of 100 microseconds each to create the
displacement and to initialize the motion. The motion was tracked with Doppler
pulses at a PRF of 5000 Hz. We processed the data using a phase shift algorithm
in real time.
Figure
1 displays plane shear waves created within a homogeneous PVA phantom (Fig. 1a)
and are propagating in opposite directions (Fig. 1b) with no fracture in the
phantom. Figure 2 displays plane shear waves created in the presence of a split
(2/3 depth long from the bottom, located at 1/5 width from the left). These
wave encounter a scattering effect at the split tip (Fig. 2a) and the shear
wave propagating towards the left encounters a phase change when it arrives at
the split edge.
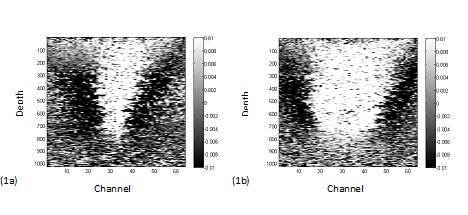
Figure 1. Plane shear waves are created within a
homogeneous PVA phantom (Fig. 1a) and are propagating in opposite directions
(Fig. 1b) with no split in the phantom.
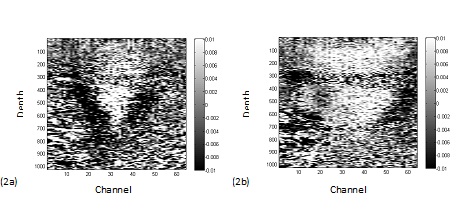
Figure 2. Plane shear waves created in the
presence of a split (2/3 depth long from the bottom, located at 1/5 width from
the left) encounter a scattering effect at the split tip (Fig. 2a) and the
shear wave propagating towards the left encounters a phase change when it
arrives at the split edge (Fig. 2b). Figure 2 provides support to our
hypothesis that shear wave elastography can image
liver fractures.