Wear Two and Call Me in the Morning –Ultrasound Enhanced Pain Relief Patches
Matt Langer – mlanger@zetroz.com
Sabrina Lewis – sabrina@zetroz.com
Shane Fleshman – sfleshman@zetroz.com
George Lewis – george@zetroz.com
ZetrOZ, Inc.
56 Quarry Road
Trumbull, CT 06611
Popular version of paper 4aBA7
Presented Thursday morning, June 6, 2013
ICA 2013 Montreal
Over the last decade, the public has become increasingly aware of the potentially dangerous, systemic side effects of pain medication. Even readily available over-the-counter drugs like acetaminophen, ibuprofen, and aspirin can cause serious damage to the digestive system as a result of long term usage and/or high dosage (Bacchi et al., 2012). A possible alternative to pills for pain relief is transdermal drug delivery, the transfer of drugs across the skin. Transdermal delivery has the advantage of keeping the drug in the area where it is applied (Yuan et al., 2009), allowing for a reduced total dose compared to a pill, but there are challenges with the method. The skin evolved as a highly efficient barrier to keep foreign substances out. After a drug gets through the skin, there is the problem of assuring drug is delivered evenly in a dose that is effective. Current transdermal drug delivery methods such as aspirin creams use chemical enhancers to allow the drugs to pass through the skin. The amount of aspirin that is absorbed by the body is still limited however and may not provide adequate pain relief. Faced with these challenges, there is a great deal of interest in researching new drug delivery methods for pain relief which are administered locally and may not have the same systemic side effects as oral medications.
A potential answer to this problem comes not from your pharmacist’s shelf, but from your physical therapist’s office: Ultrasound, or sound pressure waves that are higher frequency than can be heard by humans. Most often used for imaging tissue, ultrasound has been shown in laboratory research to improve the transference of drugs through the skin (Polat et al., 2011). Ultrasonic waves can create tiny enhanced transport pathways in the skin, through which a drug can then enter the body more quickly. The challenge with ultrasound has been finding a platform that can be used safely and easily by the general public. Research performed using ultrasound miniaturization, ultrasound coupling and the “Sonobandage” technology developed by ZetrOZ, Inc. has demonstrated the feasibility of using ultrasound to deliver pain medication through the skin.
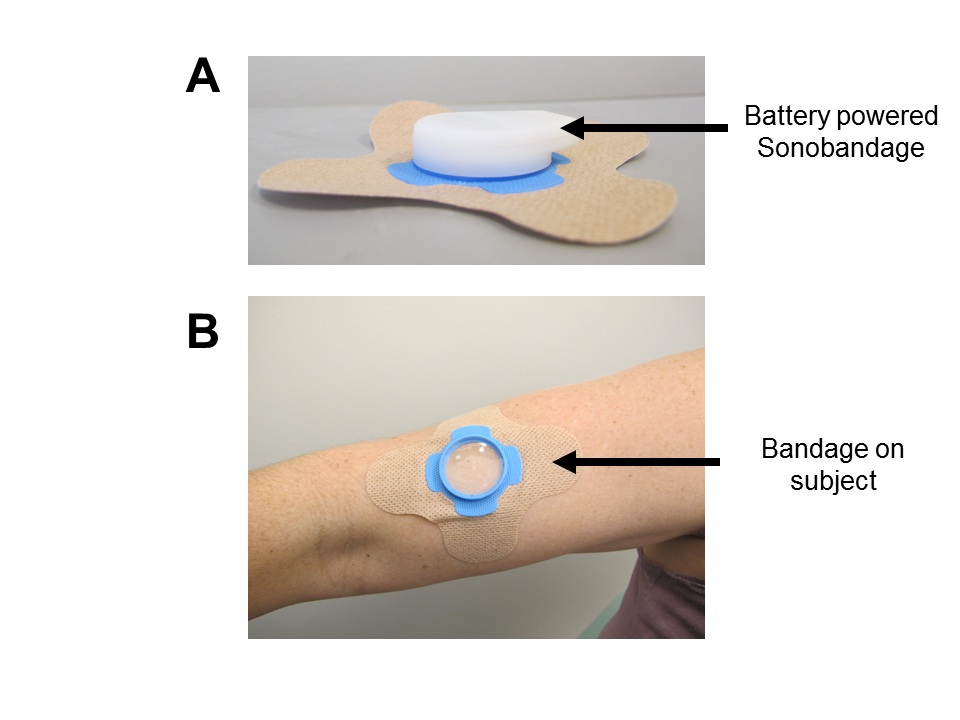
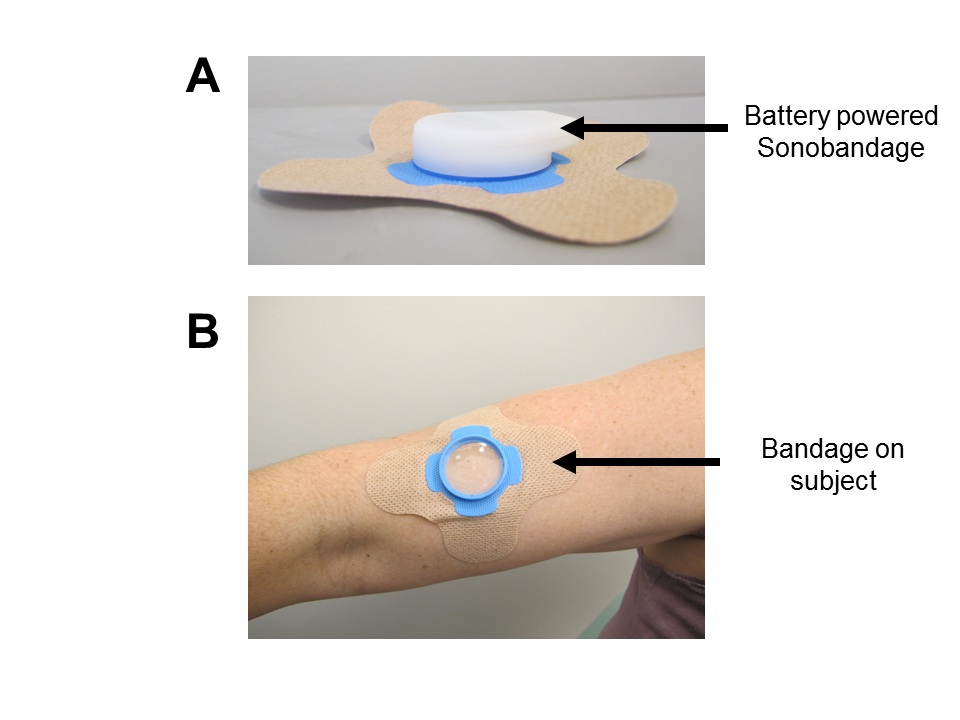
Figure 1: (A) The Sonobandage with the ultrasound device clipped into it. (B) The sonobandage, as it would appear before attaching the ultrasound device.
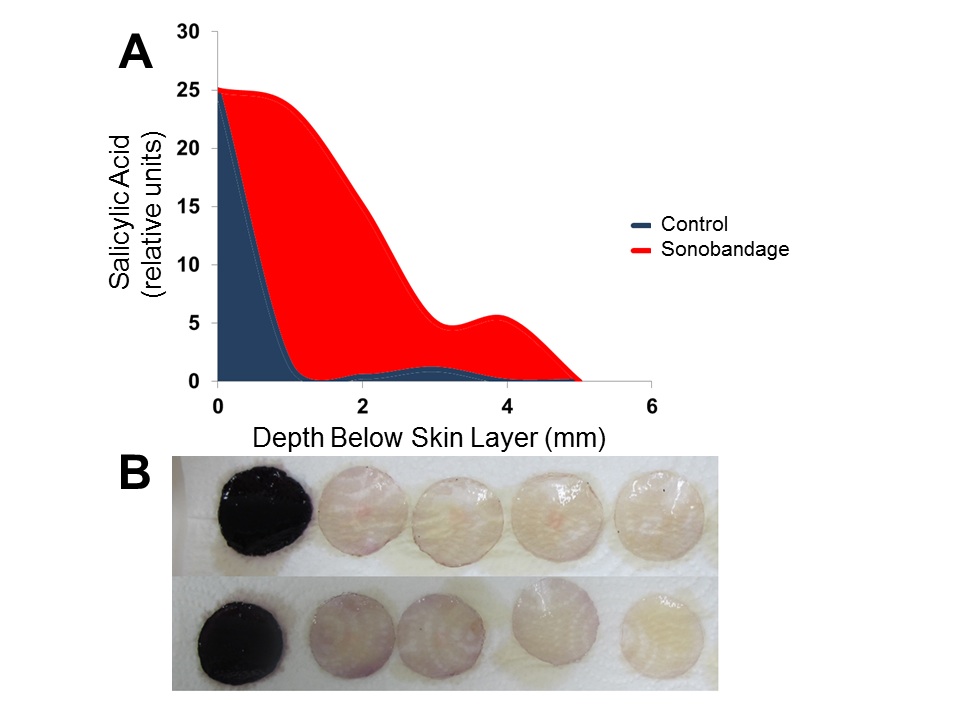
The Sonobandage uses a novel type of ultrasound gel that can be loaded with medication. The miniature ultrasound device (about the size of an iPod™ nano) clips into the Sonobandage and produces continuous oscillating sound pressure waves that deliver the medication through the skin over multiple hours. Using the Sonobandage system enhanced the ability of salicylic acid, the active form of aspirin, to cross over a bio-mimic skin model by 2400% (Figure 1). Another positive aspect of the Ultrasound Sonobandage system is that it promoted an even distribution of medication over the entire treatment volume.
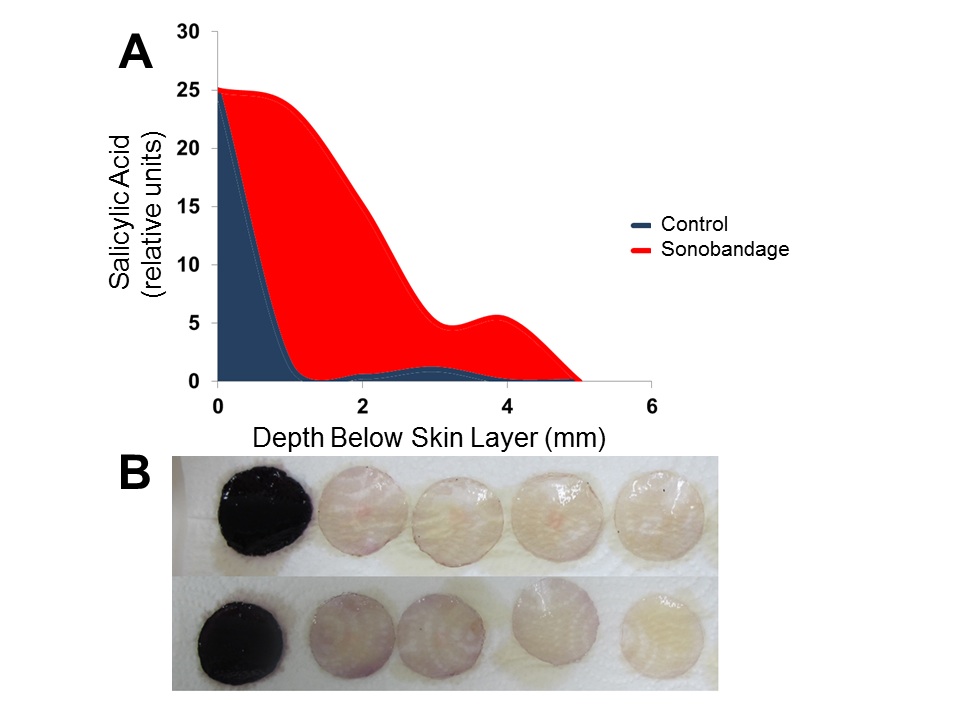
Figure 2: (A) Salicylic acid migration through a skin membrane from a source (left) into four stacked disks without ultrasound. (B) Salicylic migration through a skin-like membrane with ultrasound. Each disk on the right is darker in color than the one above it, indicating more salicylic acid.
So are you going to be wearing your pain medication anytime soon? The technology requires continued research, and will have to go through the FDA approval process. Still, it is exciting to think that in the future, localized pain relief will be achieved with localized treatment.
References
(1) Bacchi, S., Palumbo, P., Sponta, A., and Coppolino, M. F. (2012). "Clinical pharmacology of non-steroidal anti-inflammatory drugs: a review," Anti-inflammatory & anti-allergy agents in medicinal chemistry 11, 52-64.
(2) Polat, B. E., Hart, D., Langer, R., and Blankschtein, D. (2011). "Ultrasound-mediated transdermal drug delivery: Mechanisms, scope, and emerging trends," Journal of Controlled Release 152, 330-348.
(3) Yuan, Y., Chen, X.-y., Li, S.-m., Wei, X.-y., Yao, H.-m., and Zhong, D.-f. (2009). "Pharmacokinetic studies of meloxicam following oral and transdermal administration in Beagle dogs," Acta Pharmacol Sin 30, 1060-1064.