Michael V. Scanlon - mscanlon@arl.army.mil
US Army Research Laboratory
Adelphi, MD
(301) 394-3081
Popular version of paper 5pBB8
Presented Friday afternoon, December 6, 2002
First Pan-American/Iberian Meeting on Acoustics, Cancun, Mexico
The Army Research Laboratory has developed a unique body-contacting acoustic sensor that can monitor the health and performance of firefighters and soldiers while they are doing their missions. A gel-coupled sensor has acoustic impedance properties similar to the skin that facilitate the transmission of body sounds into the sensor pad, yet significantly repel ambient airborne noises due to an impedance mismatch. This technology can monitor heartbeats, breaths, blood pressure, motion, voice, and other indicators that can provide vital feedback to the medics and unit commanders. Acoustic signal processing techniques can be developed to recognize physiological events such as cough, gag, wheeze, and vomit, which may be indicators of hazardous material effects, biological or chemical weapons, or other severe medical or environmental conditions. Useful for soldiers, firefighters, and law enforcement, the sensor system can transmit physiology to remote locations for health and performance assessment. In addition to physiology, the sensor is optimally suited for monitoring speech for voice communications or automatic speech recognition for computer controls. Larger Army programs such as Land Warrior, Objective Force Warrior, and Future Combat Systems will benefit from the ability to monitor physiology, voice, and activity through sensors built into the helmet or other body-contacting hardware (see figures 1 and 2). The ARL-patented technology will benefit the commercial sector for ambulatory health monitoring.


Figure 1: Helmet, gel-sensor in suspension pad

Figure 2: Gel-sensor in neck strap
Tests were conducted to see how well the acoustic sensors monitored firefighter physiology amidst the intense activity and environment. Sensors, data acquisition hardware, and data transmitter were attached to one firefighter, who was the lead of the team and was at the nozzle of the hose. Digitized data was stored on a small body-worn computer as well as digitally transmitted to another laptop for real-time viewing. Visit www.arl.army.mil/acoustics/michael_scanlon.htm for a more detailed report on the experiment. The first part of the experiment required the firefighting team to crawl/walk through a smoke-filled two-story building to search for and rescue a mannequin (located on the second floor).Once the mannequin was brought down the stairs and outside, the firefighters then went back to where they found the mannequin and brought the hose back out. The second part of the experiment required the firefighters to enter a smoke-filled building to locate a disoriented firefighter, escort him to safety, then proceed upstairs to put out the fire.
.

Fig. 3: Disoriented fireman Fig. 4: Fire being extinguished
Fig. 5: ECG heart rate for each fireman
Figures 3 and 4 show the thermal images taken during the experiment. Figure 5 shows the ECG derived heart rate from both firefighters doing both scenarios. The ability to monitor this heart rate is an important tool, in that the duration of elevated heart rates and the maximum rate achieved can be an indicator of a firefighters ability to safely and effectively perform his or her mission. It can also be a good indicator of which firefighters are ready to reenter a building fire after a break.
Figures 6 and 7 show the gel-coupled neck acoustic sensors and its position below the hood. Two sensors were chosen for redundancy and noise canceling features. Figures 8 and 9 show how the mask acoustic sensor is attached. An acoustic sensor in the mask position picks up heartbeat pulses from the temple, breath sounds through sinus and tissue conduction, voice, coughing, wheezes, and activity. Figures 10 and 11 show the wristband acoustic sensors.



Fig. 6: Neck sensor strap Fig. 7: Sensor on Fig. 8: Mask sensor



Fig. 9: Sensor on mask
Figure 12 shows a 24-second section of data. Channels 1 and 2 are the left and right acoustic neck sensors, channels 3 and 4 are the left and right acoustic wrist sensors, channel 5 is the boom microphone, channel 6 is the acoustic mask sensor, channel 7 is the Polar heartbeat indicators with a DC voltage shift superimposed for temperature, and channel 8 is the ECG signature. Alternating wrist activity is present in this data, and is indicative of the firefighters hand usage during crawling on the floor. The mask physiology is often lost due to firefighters turning their heads, and resulting motion of the breathing hose, mask, and helmet were transmitted through the mask straps to the sensor. Notice also the ECG suffers from motion artifacts during the intense motion sections. The data in figure 12 shows clear acoustic heart signals with distinct peaks for determining the inner-beat-intervals (IBIs). How the IBIs fluctuate on a beat-by-beat basis, as well as long-term trends, is termed heart rate variability (HRV) and gives an indication of how well the body is regulating blood pressure, breathing, and core temperature. These IBIs also can indicate mental activity related to concentration on a task.
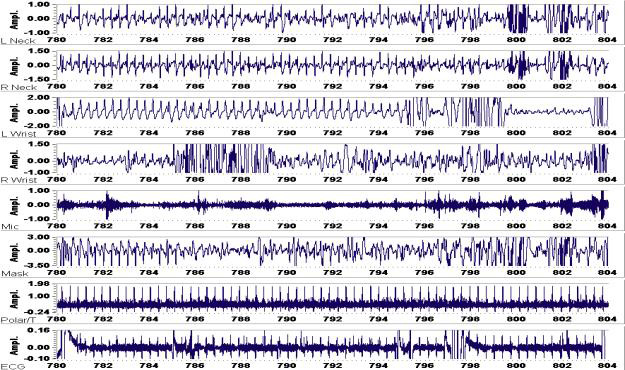
Fig. 12: Twenty-four seconds of data (top-to-bottom: L/R neck AC, L/R wrist AC, mic, mask AC, polar, ECG)
Figure 13 shows two seconds of data with clear indications of heartbeat time-difference-of-arrivals between the ECG and the neck and wrist acoustic pulses. Changes in the pulse-transit time (PTT) are directly proportional to changes in the systolic blood pressure. The time it takes for the pulse to travel between two fixed locations (such as from the heart to the wrist) is directly proportional to the pressure of the blood (speed of sound in the artery changes with respect to density and the velocity component of the blood flow). By measuring the time-difference between the heartbeat indications from variations of ECG-neck, ECG-wrist, ECG-head, neck-wrist, head-wrist, and neck-head, one can approximate the systolic blood pressure on a beat-by-beat basis.
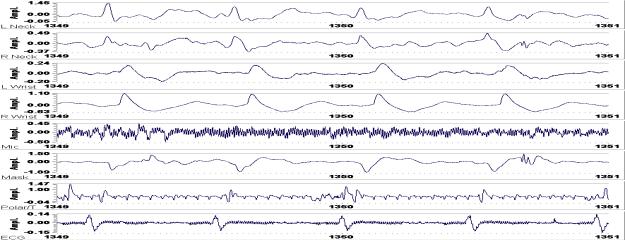
Fig. 13: Two seconds of computer stored physiology
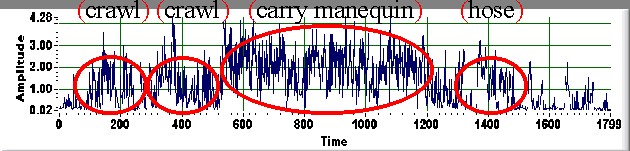
Fig. 14: RMS energy of left wrist sensor (30 minutes)
Figure 14 shows a 30-minute time history of short-duration energy calculations from an acoustic sensor on the wrist. The root-mean-squared (RMS) energy is a good estimation of how active a firefighter or soldier is. When a firefighter collapses due to injury, the signal-to-noise ratio of the physiology improves greatly due to a decrease in activity. Figure 15 shows a time waveform and associated time-frequency representation (spectrogram) of 80-seconds of data during a simulated unconscious firefighter. The first 20-seconds show him walking, standing, and then getting into position on the ground. He then holds as still as possible for approximately 40-seconds to produce excellent heartbeat and breath indications, then he gets up off of the ground.
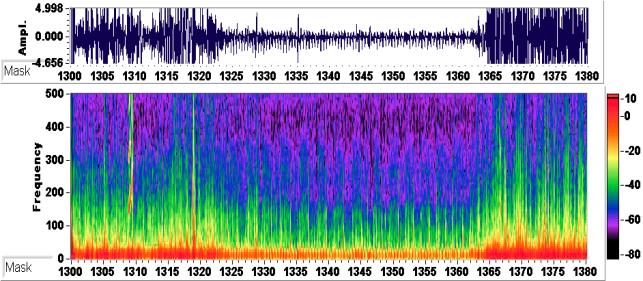
Fig. 15: Spectrogram and time-series of mask data during unconscious scenario
Acoustic sensors and signal processing can extract much information about the soldiers firefighters health and performance, as well as how they are interacting with their environment. When the person being monitored ceases to be active or during resting periods the acoustic SNR is exceptional for monitoring physiology. This is when vital signs monitoring is most important. The same gel-sensor can be used for high-quality voice communications and vital signs surveillance, thereby eliminating the need for redundant physiological and communications sensors. The gel-coupled acoustic sensors can detect very diverse physiology, and can be easily adapted/upgraded through software/algorithm modifications for many different types of monitoring applications.