Adrianus.J.M. Houtsma (Adrianus.Houtsma@us.army.mil) and
Ian P. Curry
US Army Aeromedical Research Laboratory
Fort Rucker, AL
36362-0577
John M. Sewell and William N. Bernhard
Active Signal
Technologies, Inc.
Linthicum Heights, MD 21090
Popular
version of paper 5pBB2
Presented Saturday afternoon, December 2, 2006
4th ASA/ASJ Joint Meeting, Honolulu, HI
1. INTRODUCTION
There are many medical emergencies where patient examination with a stethoscope (auscultation) is of critical importance for the patient’s survival. In military settings, medical evacuation from the battle field by helicopter (during the “critical hour”) often involves casualties with acute injuries to heart and lung function. Auscultation is an important tool for assessing the integrity of heart muscle, valves, and major arteries while blood pressure may be determined in conjunction with a pneumatic cuff. Auscultation of the lungs can be essential when confirming the placement of endotracheal tubes or when diagnosing conditions such as a collapsed lung, asthma, or pulmonary edema. Fixed-wing medical transport flights are often of longer duration, and auscultation of body sounds becomes valuable in managing chronic conditions. The environment itself may lead to further medical complications; expansion of intestinal gases at high altitudes can be monitored by auscultation of bowel sounds. Rotary-wing and fixed-wing aircraft tend to be very noisy. Without doubt there would be great benefit to accurate, easy auscultation in the noisy medical transport environment.
There are also non-military situations where auscultation in noisy environments can be an issue. Train wrecks or multiple-car highway accidents are examples where victims are often transported to hospitals in helicopters. Noisy public events like football games or pop concerts are scenes where it could be difficult for a physician to provide the right diagnosis and emergency treatment to a heart attack victim.
Conventional acoustic stethoscopes are sensitive to noise from the immediate environment because it can invade the stethoscope in at least three different ways. It can enter through the earpieces, since these always have a finite amount of sealing power. It can enter through the acoustic tubing, since sound is always conducted through the tubing walls to some extent. The most sensitive entry point is the acoustic sensor, where environmental noise enters either directly through the housing or indirectly as a surface wave propagating along the skin of the patient. As a result, the maximum noise level in the environment that still allows successful auscultation is between 80 and 85 dB sound pressure level (SPL) , dependent on details of stethoscope design and physician’s skill.
Modern electronic stethoscopes have raised the maximum tolerable environmental sound level to about 90-95 dB SPL. This is because ear pieces are replaced by insert loudspeakers that provide a better seal with the ear canal, and tubing is replaced by electrical cables that do not pick up acoustic noise. Transducers in the stethoscope head can be designed to optimize mechanical to electrical transduction of body sounds while minimiz-ing transduction of air-born sound from the environment.
Modern electronic stethoscopes are, unfortunately, still inadequate for effective auscultation in brutal noise environments as described above. Noise levels in heavy-duty helicopters like the Black Hawk can go as high as 120 dB SPL. Noise levels at indoor sporting events and pop concerts can easily reach 100 dB SPL. To conquer these high noise levels, a totally different technology was added to the stethoscope design. In ultrasound imaging, a high-frequency (megahertz range) sound signal is generated, transmitted from the stethoscope head into the patient’s body, and reflections from moving body tissue are picked up by a receiver also located in the stethoscope’s head. Since these reflections have a slightly different frequency than the transmitted signal caused by the Doppler effect, a difference-frequency can easily be computed and made into an audible sound. The advantage of this technique is that environmental noise, no matter how intense, does not interfere with the heart or lung sound, since the latter is carried by a 2.3 MHz carrier signal and a helicopter, ambulance, or stadium crowd do not produce any interfering sound at this high frequency.
There are significant differences between the sounds produced by a conventional and by an ultrasound-based stethoscope. That is because they are based on totally different physical principles, and represent different physiological processes. Where a conventional stethoscope yields a “lub-dub” sound for normal heart beat, the same heart beat heard through an ultrasound stethoscope will yield a “ta-dá-da” pattern. Because of these differences, the new noise-immune stethoscope was designed on a hybrid two-in-one principle, where a conventional operation mode can be selected for quiet or moderately noisy environments, and ultrasound opera-tion is selected in extreme noise conditions.
2. STETHOSCOPE DESIGN

The new stethoscope is shown in Fig. 1. The top part of the device is the battery compartment, containing two 1.5V AA-cells. The device can be held between the index and middle fingers, with the thumb being free to operate a 4-button control panel. The finger space has been designed to fit an average hand covered with a standard UH-60 aviation glove.
The bottom part contains the stethoscope sensors and the signal-processing electronics. For electromechanical operation, a stack of conventional piezoelectric disk elements is driven by a movable piston at the bottom (the “head’’) of the device, designed as a mechanical transformer between chest tissue of the patient and the piezo-electric stack. The purpose of this transformer is to maximize the mechanical energy transfer from the human body to the sensor stack, while minimizing energy transfer from air-born sound to the sensor stack. An O-ring, placed on the bottom surface of the stethoscope and surrounding the sensor, keeps out surface waves that can be excited on the patient’s skin by high-level environment noise or vehicle vibration.
For ultrasound operation, two semicircle-shaped disks, made of piezoelectric material, are embedded in the sensor head, where one functions as a transmitter and the other as a receiver of high-frequency sound waves. For this mode of operation, a contact gel placed between the stethoscope head and the patient’s skin must be used to minimize ultrasound reflections at the sensor-skin boundary.
A thumb-operated 4-button control panel allows the device to be turned on, the signal volume to be set, and the operating mode to be selected. This allows a physician to switch between modes during auscultation of a patient, as long as noise levels are not so high as to obscure conventional-mode auscultation. Switching could be important, since each mode of auscultation provides its own specific kind of information. The stethoscope has a single signal output jack that can feed a set of Communications Earplugs ® or other types of sealed insert earphones or headsets.

Figure 2.
Stethoscope connected to Communications Earplugs and tube of ultrasound contact
gel.
Heartbeat auscultation was performed by a trained physician on a single healthy male subject of average body size. The auscultation environment was a reverberant chamber, equipped with high-power sound equipment capable of producing UH-60 type noise of various intensity levels, and yielding an approximately diffuse sound field. The maximum intensity level that could be produced by the sound system was 120 dB SPL.
The stethoscope was connected to a set of Communications Earplugs (CEPs) as shown in Fig. 2. With the earplugs inserted (providing one layer of environmental noise protection), the auscultating physician wore a standard HGU-56/P aviation helmet equipped with circumaural ear pads, providing a second layer of environmental sound attenuation. For comparison with a conventional acoustic 3M Littmann Cardiology III stethoscope, one ear piece of the Littmann was plugged to prevent environmental noise to enter the system, while the other ear piece was acoustically coupled to a Brüel & Kjær Type 4134 condenser microphone. This transformed the Littmann temporarily into an electronic stethoscope, yielding an electrical output signal.
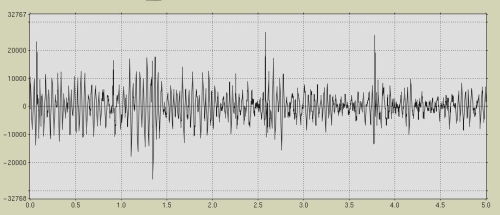
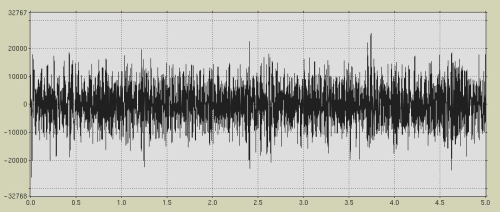
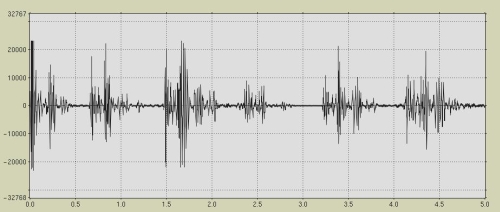
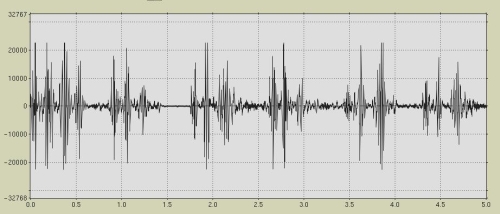
Digital recordings of heartbeat signals were made at 16-bit resolution and 8-kHz sampling rates, at background noise levels from 70 to 110 dB SPL in 5-dB steps. A selection of results, obtained at background noise levels of 70 and 100 dB SPL are shown in Fig. 3. Graphs represent 5-second samples of stethoscope output on an arbitrary linear amplitude scale. Figure 3a, taken from the Littmann, shows a clearly discernable and audible heartbeat at 70 dB noise and a totally obscured and inaudible heartbeat at 100 dB. Figure 3b, however, shows almost identical heartbeat signals for the 70 dB and 100 dB background noise conditions, with both signals being clean and clearly audible. Even in a background noise level of 120 dB SPL, the maximum that could be produced by the equipment, the ultrasound stethoscope’s output remained essentially noise-free.
Conventional passive acoustic stethoscopes are ineffective in noisy environments that exceed levels of 80-85 dB SPL. Even if noise-attenuating earmuffs are worn, with the stethoscope tubing being fed through the earmuff walls, the background noise would still invade the system through the stethoscope’s sensor head.
Ultrasound technology offers an auscultation mode that is essentially free of acoustic noise invasion from the environment. Auscultation in very noisy environments using this technology is limited only by the amount of hearing protection worn by the physician and by the maximum amount of sound that can be tolerated by the human ear. There always is, of course, some system noise associated with physical movement in the placement or orientation of the stethoscope head. This explains why measured signal-to-noise ratios in the output signal are not infinite but typically limited to about +20 dB.
Finally, the use of ultrasound in auscultation offers other advantages besides providing an essentially noise-free signal. The signal also contains information that cannot be obtained with conventional acoustic or electro-mechanical stethoscopes. Ultrasound acoustic images contain artifacts of tissue movement that could be of interest to cardiologists or other specialists, if it can be shown that specific sound features are correlated with specific physiological anomalies. Such exploration is left for future research.
DISCLAIMER
Opinions, interpretations, and conclusions contained in this article are those of the authors and are not necessarily endorsed by the U.S. Army and/or the Department of Defense.