1aBAb12 – Novel use of a lung ultrasound sensor for monitoring lung conditions
Novel use of a lung ultrasound sensor for monitoring lung conditions
Tanya Khokhlova – tdk7@uw.edu
Adam Maxwell – amax38@uw.edu
Gilles Thomas – gthom@uw.edu
Jeff Thiel – jt43@uw.edu
Alex Peek – apeek@uw.edu
Bryan Cunitz – bwc@uw.edu
Michael Bailey – mbailey@uw.edu
Kyle Steinbock – kyles96@uw.edu
Layla Anderson – anderla@uw.edu
Ross Kessler – kesslerr@uw.edu
Adeyinka Adedipe- adeyinka@uw.edu
University of Washington
Seattle, WA, 98195
Popular version of paper ‘1aBAb12 – Novel use of a lung ultrasound sensor for detection of lung interstitial syndrome’
Presented Monday morning, November 29, 2021
181^st ASA Meeting
The need to continuously evaluate the amount of fluid in the lung is essential in patients suffering from a number of conditions, including viral pneumonia (including COVID-19) and heart failure, and patients on dialysis. Chest x-ray and CT are typically used for this purpose, but can not be done continuously due to the radiation dose, and have logistical limitations in some cases, for example when transporting unstable patients or patients with COVID-19 due to the risk of contagion. Lung ultrasound (LUS) is non-ionizing and safe, and has recently emerged as a useful triage and monitoring tool for quantification of lung water. Because lung is air-filled, it is reflective for ultrasound, and in LUS exams it is image artifacts that are being evaluated, rather than true lung images. The artifacts termed A-lines are periodic bright horizontal lines parallel to the lung surface representing multiple reflections of ultrasound pulse from the lung and indicating a normal aeration pattern. The artifacts termed B-lines are comet-like bright vertical regions originating at the lung surface and extending down. The number and distribution of B-lines are known to correlate with presence of fluid in the lung and the condition severity. However, visualization and quantification of B-lines requires training and is machine and operator dependent, whereas in select clinical scenarios continuous, automated hands-free monitoring of lung function is preferred, e.g. COVID19 infection.
In this study we were aiming to identify the detected ultrasound signal features that are associated with B-lines and to develop a miniature wearable non-imaging lung ultrasound sensor (LUSS). Individual adhesive LUSS elements could be attached to patients in specific anatomic locations similarly to EKG leads, and ultrasound signals would be collected and processed with automated algorithms continuously or on demand. First, we used an open platform ultrasound imaging system to perform standard 10-zone LUS in ten patients with confirmed pulmonary edema, and in five healthy volunteers. The ultrasound signal data corresponding to each image were collected for subsequent off-line Doppler, decorrelation and spectral analyses. The metrics we found to be associated with the B-line thickness and number were peaks of Doppler power at the pleural line and the ultrasound signal amplitude corresponding to a large depth.
Left: examples of lung ultrasound images containing A-lines and B-lines and the corresponding signals detected by the ultrasound imaging probe. Right: conceptual diagram of the use of LUSS for monitoring of lung condition and a prototype LUSS element. Adhesive LUSS elements are applied in 10 anatomic locations and automated signal processing software displays lung fluid score for each element on a 4-point scale: none (green), mild (yellow), moderate (orange) or severe (red).
Next, we built miniature LUSS elements powered by custom-built multiplexed transmit-receive circuit, and tested them in a benchtop lung model – polyurethane sponge containing variable volumes of water – side by side with LUS imaging probe previously used in patients. Wetting of the sponge produced B-lines on the ultrasound images, and the associated ultrasound signals were similar to those measured by LUSS elements. We hope to proceed with testing LUSS in human patients in the nearest future. This work was supported by NIH R01EB023910.







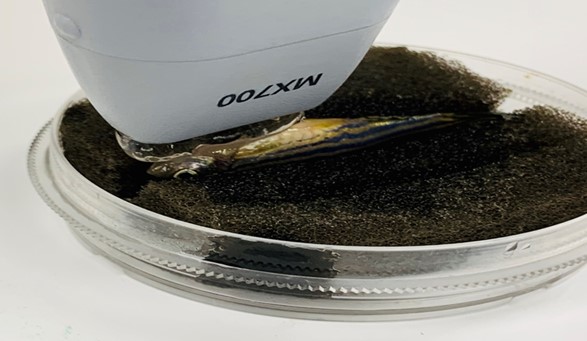 Figure 1. Experiment setup of zebrafish echocardiography.
Figure 1. Experiment setup of zebrafish echocardiography. Figure 2. Experimental setup of zebrafish ultrasound vibro-elastography.
Figure 2. Experimental setup of zebrafish ultrasound vibro-elastography.