1pBAb5 – Predicting Spontaneous Preterm Birth Risk is Improved when Quantitative Ultrasound Data are Included with Prior Clinical Data
Barbara L. McFarlin, bmcfar1@uic.edu
Yuxuan Liu
Shashi Roshan
Aiguo Han
Douglas G. Simpson
William D. O’Brien, Jr.
Popular version of 1pBAb5 – Predicting spontaneous preterm birth risk is improved when quantitative ultrasound data are included with prior clinical data
Presented Monday afternoon, November 29, 2021
181st ASA Meeting
Click here to read the abstract
Preterm birth (PTB) is defined as birth before 37 completed weeks’ gestation. Annually in the U.S., more than 400,000 infants are born preterm, and over 1 billion globally. Consequences of PTB for survivors are severe, can be life-long and cost society $30 billion annually, a cost that far exceeds that of any major adult diagnosis. Predicting women at risk for sPTB has been medically challenging due to 1) lack of signs and symptoms of preterm labor until intervention is too late, and 2) lack of screening tools to signal sPTB risk early enough when an intervention would likely be effective. Spontaneous preterm labor is a syndrome associated with multiple etiologies of which only a portion may be associated with cervical insufficiency; however, regardless of the reason of PTB, the cervix (the opening to the womb) must get ready for birth to allow passage of the baby.
Our Novel quantitative ultrasound (QUS) technology has been developed by our multidisciplinary investigative team (ultrasound, engineering and nurse midwifery) and shows promise of becoming a widely available and a useful method for early detection of spontaneous preterm birth. Our preliminary results of 275 pregnant women who received two ultrasounds during pregnancy, determined that QUS improved prediction of preterm birth and was an added feature to current clinical and patient risk factors. QUS technology is a feature that can readily be added to current clinical ultrasound systems, thereby reducing the time from basic science innovation translation to improve clinical care of women.
This research was supported National Institutes of Health grant R01 HD089935







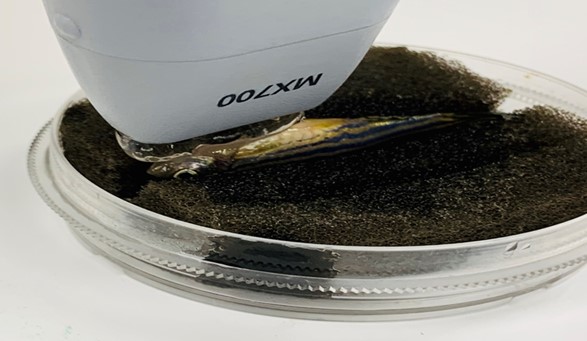 Figure 1. Experiment setup of zebrafish echocardiography.
Figure 1. Experiment setup of zebrafish echocardiography. Figure 2. Experimental setup of zebrafish ultrasound vibro-elastography.
Figure 2. Experimental setup of zebrafish ultrasound vibro-elastography.